Emergency Department Improvements Using Collaboration & Lean Practices
A hospital chain hired me to work with their directors and the physicians’ group to develop a strategy for improving patient satisfaction and reducing left without being seen (LWBS).
After completing assessments at each of their five emergency departments (ED), we hypothesized that Patient Satisfaction and LWBS would improve if we reduced the length of stay (LOS). The team agreed we should start at the hospital with the most issues. The staff at this hospital was exhausted, and the waiting room was constantly filled. During an assessment, a nurse began crying at this site because she and others felt hopeless.

Emergency Department Entrance
The team agreed we would work on lower acuity patients since this made up most patients entering the hospitals. We selected acuities 3, 4 & 5. Patients with acuities 3, 4 & 5 would likely not be admitted to the hospital.
The team also agreed that the top 3 items to address were:
- Flow in and out of the ED rooms.
- Building a collaborative team that met regularly and shared data.
- Reducing write-offs.
We chose these three because improving one would improve the other two items.
Our time studies and observations showed we could improve flow if we moved patients out of the room almost immediately after seeing the physician. The physician statistically sees patients with these acuity levels for less than 20 minutes, except when triage misidentifies a patient.
In the past, hospital administrators believed that patient satisfaction would be higher if patients were kept and discharged in the same ED room.
Should a patient need any scans, imaging, or laboratory work, patients may or may not be permitted to stay in the ED room. Sometimes patients were sent elsewhere, and the registrars could not capture the government and financially required information, which caused write-offs.
Before we could change the department’s choreography, we needed to work on sacred cows and business models.
We met with the hospital’s senior leadership and requested that we move patients after seeing the physician for acuities 3, 4 & 5 rather than stay in the ED room. We wanted to create a standard operating procedure for all these patients.
The team requested that some rooms be kept open, just for acuities 3, 4 & 5, except for higher acuities 1 & 2.
The physicians, hospital administrators, nursing directors, and other clinicians agreed to meet every other week. We also decided to create a dashboard showing our progress.
The team requested that IT change the tablets for the scribes assigned to physicians. When the scribe hit “send notes,” an alert appeared on the registrar’s laptop. This told the registrar the physician was done, and they had 5 minutes to get the needed data. We strategically located the registrar’s workstations. They could now see all the ED rooms and get to them quicker.
After the registrar completed their task, the patient was sent or escorted to the next step in their recovery.
As soon as the patient left the room, it was cleaned and prepped for the next patient. The goal was to turn the room around in 20 minutes.
To improve the accuracy of determining acuity, we altered the triage process so that any errors were on the side of caution. We changed the triage questions to identify potential sepsis patients.
When patients were tested, imaged, etc., they returned to the ED. However, they were placed in an area specifically used for consultation and discharge.
The practice of always having the same physician discharge a patient was also changed, as most of these patients could be discharged by another physician or qualified staff.
Outcomes:
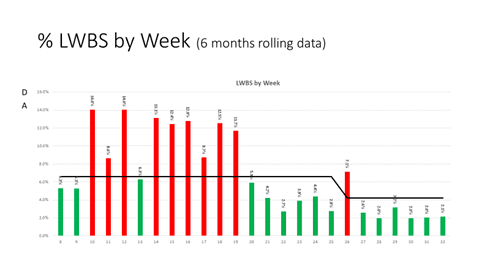
Left Without Being Seen dropped from an average of 10.8% before the new process to 2.4%. With an increase in traffic of 11.3%.
The new triage practice helped patients get their lab results often before being seen by the physician, reducing the length of stays by over 60 minutes for those patients.
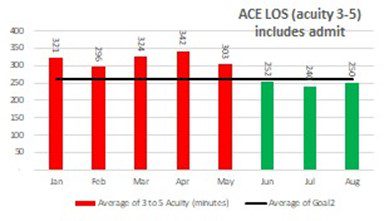
The length of stay for acuities 3, 4 & 5 was reduced from 314 to 249 minutes.
The hospital recognized an estimated additional $8.6M in revenue.
Write-offs fell to $0. The hospitals had $637K in losses in the prior six months.
The dashboards provided stack-up information throughout the patient’s journey and identified wait times and the reasons. This data allowed the team to focus on the areas causing longer stays.
The data also showed what equipment was being utilized, avoiding the purchase of $1.6M in imaging equipment as it was determined that the current equipment had less than 15% utilization.
After we launched the new processes, one of the Physicians stated that things were improving because there was less traffic into the ED. I opened the dashboard and showed her that she and her colleagues saw 11% more patients. She stated that it seemed much more manageable and assumed fewer patients.
I could not get patient satisfaction data because this data lagged by a couple of months, and my assignment ended before the data could be correlated with the length of stay.
The most gratifying thing for me was watching the staff enjoy performing their tasks, even on busy days.
Recommendations:
The lean tools were the same as most projects involving flow. The critical process was in the observations. It was a real asset to have personnel conduct observations who understood the processes, the medical terminology, and the roles everyone plays. Always have “smart” team members who know the processes and want change.
Lean into addressing opposing business practices. The hospital would not provide added nursing support unless there were more physicians. The physicians’ group would not place more doctors unless they had more supporting staff. The remedy was getting everyone at the table and agreeing to try the new process and test our hypothesis.
The hospital and physicians brought in the added staff to test our hypothesis. On the first test day, the physicians saw almost 50% more patients, and the length of stay dropped by over 36%.
Re-test your hypothesis. We did this by removing the added support but kept the process we developed. We saw an increase in the length of stay, but not as bad as before the changes. From this, we determined that staffing could be adjusted if there were significant swings in traffic. This would be helpful if staffing were needed in other parts of the hospital more than the ED.
Recognize that nurses, physicians, clinicians, and staff are well-trained and work hard. They have challenging tasks they perform. Listen to them, use their terminology, and understand they will want to improve, but on their terms.
Finally, don’t chase everything wrong before testing your hypothesis. We used a diagnostic tool that tied the combined teams’ core values and set our priorities. This tool helped eliminate any discussions on what was important.
To get copies of the tools used, contact Stockman Strategic Solutions. We will be glad to share out tools and methods.
